What Are IVF Success Rates By Age
What Are IVF Success Rates By Age
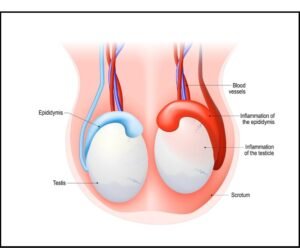
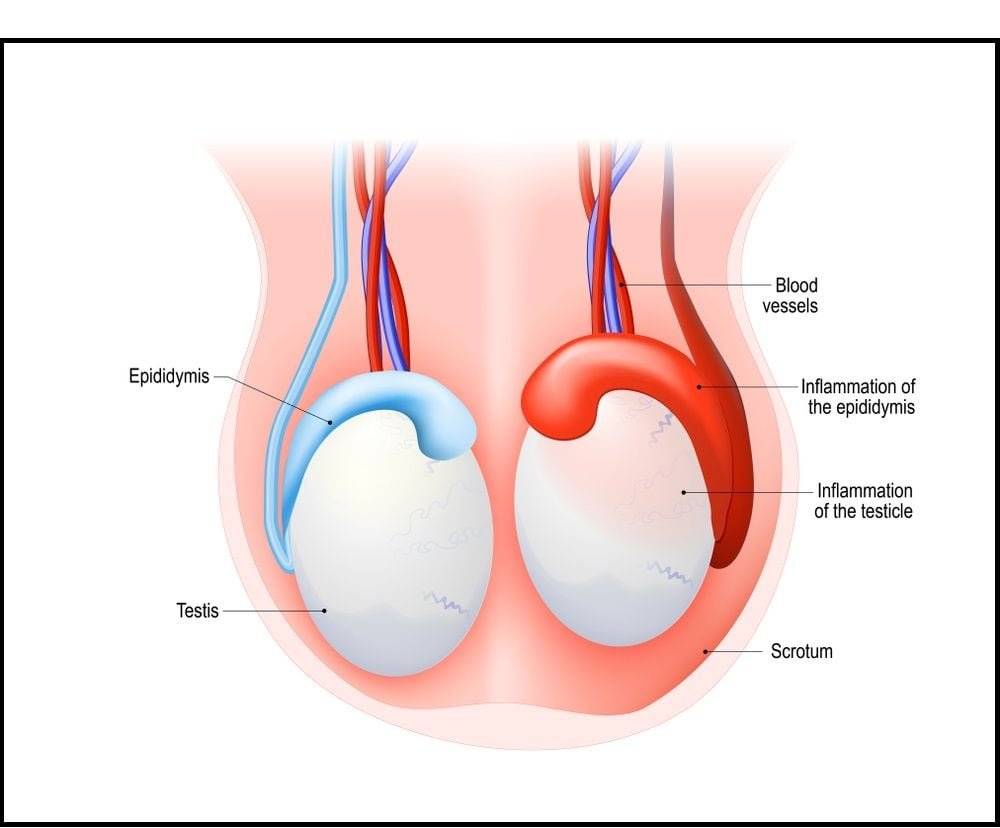
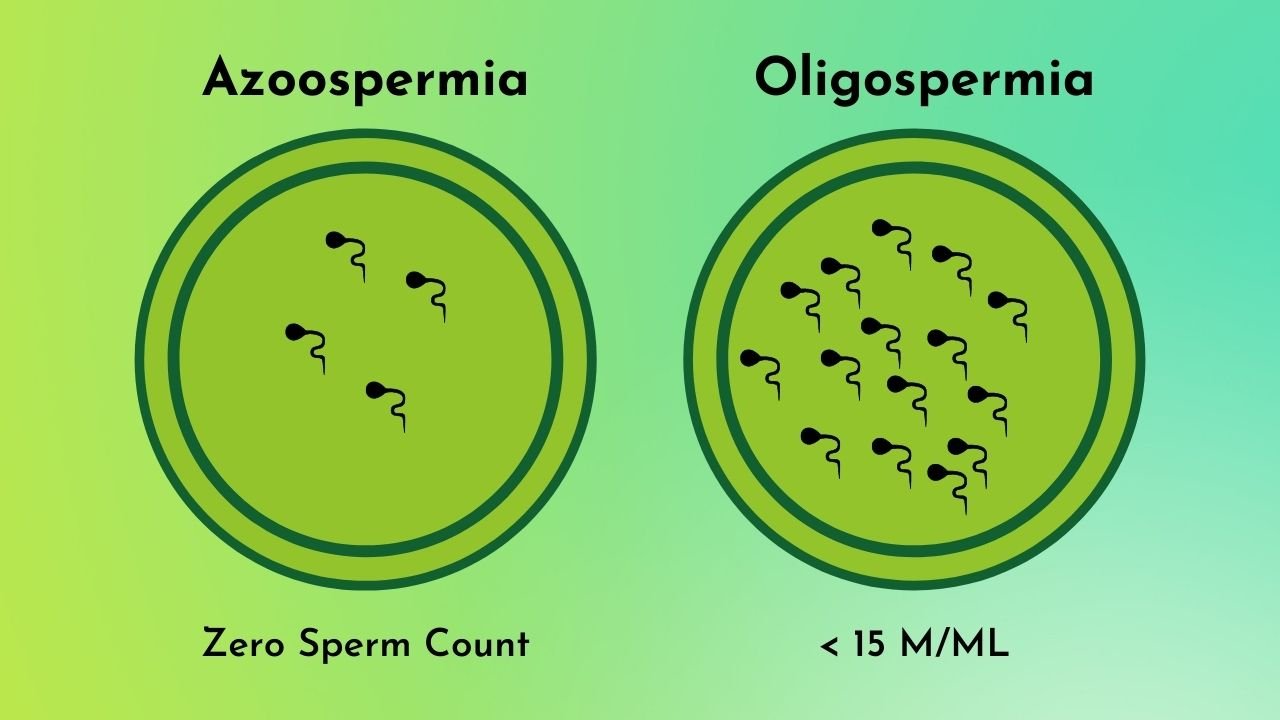
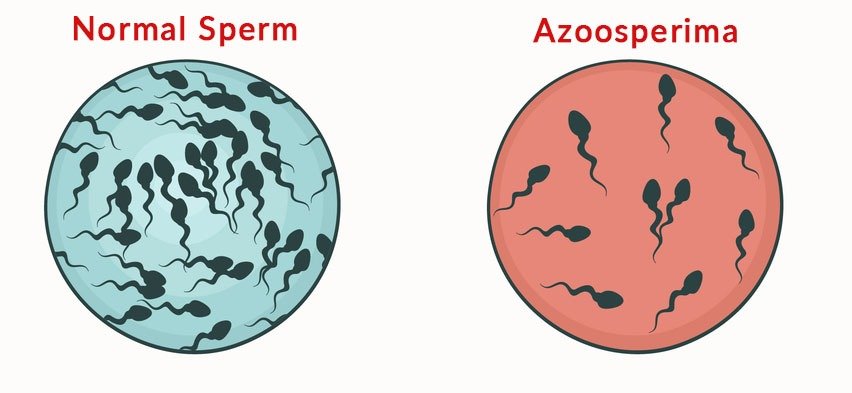
IVF (in-vitro fertilization) is an effective assisted reproductive technology that helps partners conceive. The technology works for couples diagnosed with infertility because of various factors, including blocked fallopian tubes, endometriosis, congenital uterine anomalies, etc., in women, and azoospermia, genetic problems, and immune problems in men.
Many things affect one’s ability to conceive, one of which is maternal age. According to a report by the Centers for Disease Control and Prevention, the average age of a woman getting pregnant for the first time is 27.
While IVF can help partners struggling with infertility, its success rate depends on your age.
In this post, we’ve shared the IVF success rate by age, factors affecting the success of IVF treatment, and the best age for a woman to consider the procedure. Read on.
When Should You Consider IVF?
Negative pregnancy test results after trying for a year or longer to conceive indicate a problem with your fertility. Reasons why a couple might choose IVF include blocked or damaged fallopian tubes, endometriosis, uterine fibroids, PCOD, and low egg reserve (to name a few). IVF also works in cases of male infertility.
IVF is considered a step ahead of regular fertility treatments. If you have tried all medications, surgical procedures, and hormonal treatments but have seen no results, IVF is your best chance at conceiving.
In-vitro fertilization isn’t only for couples who can’t conceive naturally, but it’s advised for those who fear passing their problematic genes to their children. The procedure involves Preimplantation Genetic Screening (testing the embryo for genetic problems before they are implanted into the uterus). This makes it a safer choice for parents with genetic disorders.
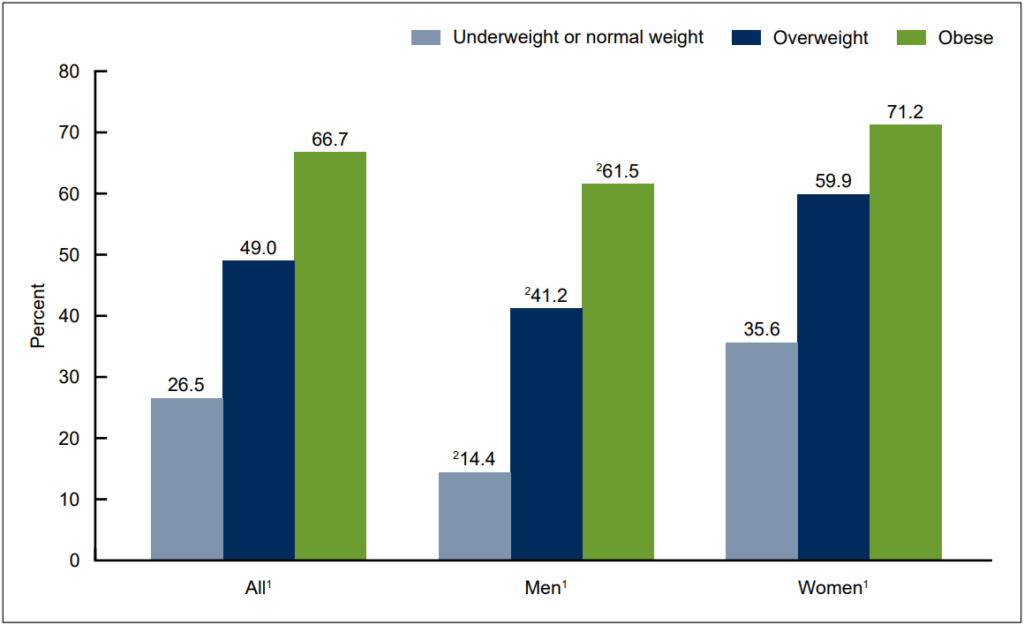
IVF Success Rate By Age
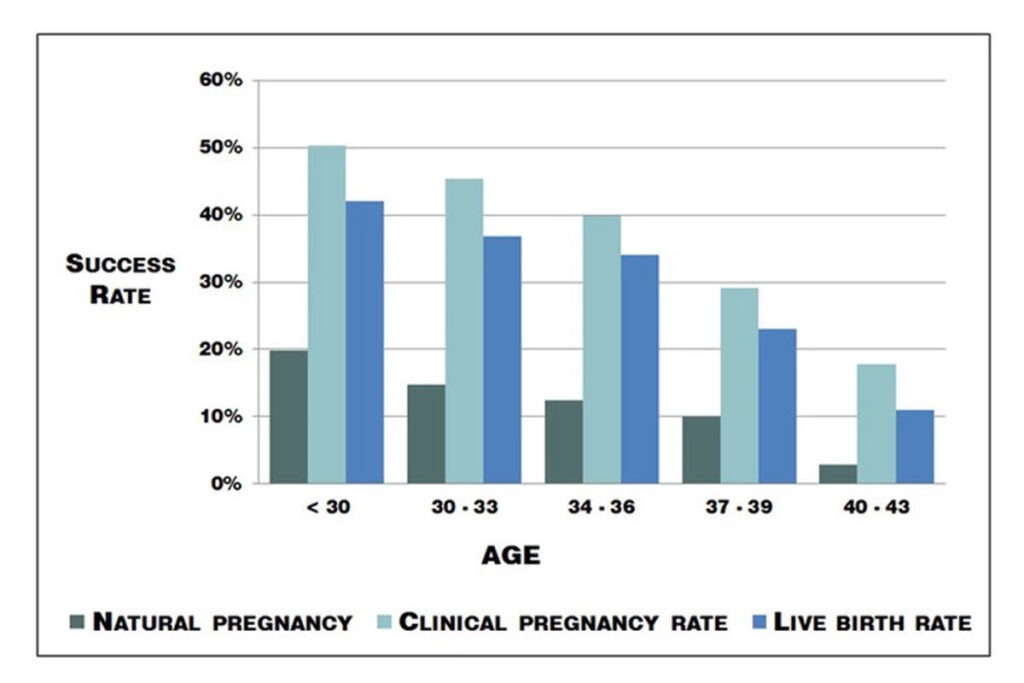
This happens because a woman’s egg reserves and quality decline after a certain age, affecting her ability to conceive naturally.
According to SART’s reports, the IVF success rate by age is shown below.
- Under 35
- Age 35-37
- Age 38-40
- Age 41-42
- Above 42 years
Woman’s Age
- 44.5%
- 32.4%
- 20.2%
- 9.6%
- 2.9%
IVF Success Rate
Can You Get Pregnant On the First Try?
Some women achieve a healthy and viable pregnancy on the first attempt of the IVF cycle. Younger women are likely to conceive quickly because of the good egg supply. The chances increase if you opt for multiple embryo transfers, but that comes with the risk of multiple pregnancies.
How Does Your Age Affect Your Fertility?
Even if a woman conceives at an older age, she has a higher risk of pregnancy-related complications than a younger woman. The chances of miscarriage and genetic abnormalities (due to poor egg quality) increase after 35. There’s also an increased risk of preeclampsia, gestational diabetes, placenta previa, and stillbirth in older women.
What Factors Affect the IVF Success Rate?
- Your general health
- Your uterine anatomy
- Your AMH levels
- Your uterine lining
- Sperm count and quality in men
- The number and quality of eggs retrieved
The lower your AMH level, the fewer eggs your healthcare provider can retrieve. Before in-vitro fertilization treatment, you will undergo a series of tests that evaluate your uterine anatomy, AMH levels, and overall reproductive health.
How to Improve IVF Success Rate?
No supplement can magically increase your pregnancy success rate after an IVF cycle. However, experts recommend a few tips to improve your chances of conceiving. This applies to both—women who conceive naturally and those undergoing IVF or other assisted reproductive treatments. Here’s what can help:
- A Healthy Weight: Overweight and obese women face more complications in getting and maintaining pregnancy than healthier women with a normal body mass index. That’s because your weight affects your ovulation cycle and causes hormonal imbalance.
- Quit Alcohol and Smoking: Smoking cigarettes has been linked to poor egg quality in women. Likewise, alcohol consumption can negatively affect your pregnancy.
- Improve Your Dietary Intake: Add lots of vitamins, minerals, and healthy nutrients to your diet. Limit the intake of caffeine, processed foods, and other unhealthy snacks.
What Should You Expect During IVF?
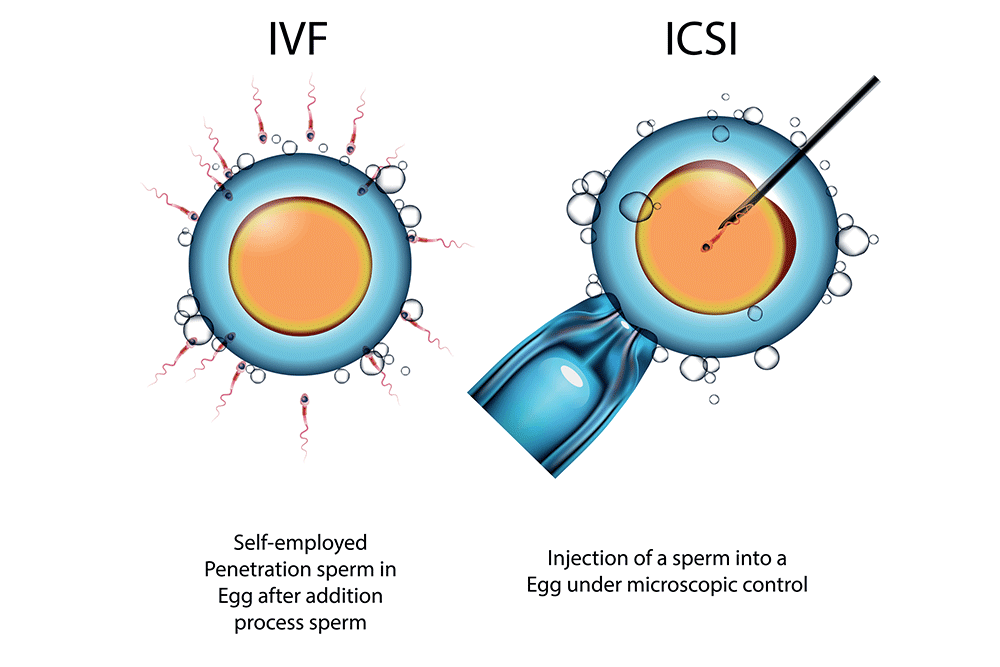
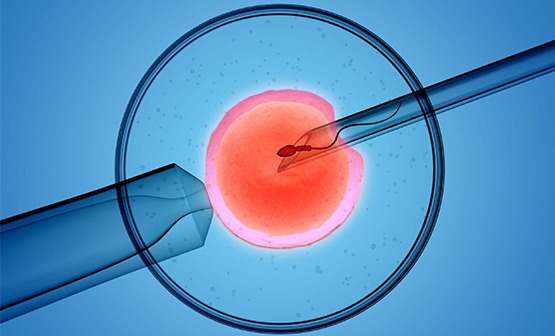
IVF is divided into five stages, starting with the ovarian stimulation. Your doctor will give you hormonal injections to stimulate the production of eggs. They will schedule egg retrieval, in which the mature eggs are collected from your ovaries and are mixed with the sperm in an incubator. They are left overnight for fertilization. The fertilized eggs are transferred into the woman’s uterus through a minimally invasive procedure.
Pregnancy Through Other Assisted Reproductive Technology
IUI – Intrauterine Insemination is another procedure that helps women achieve a healthy pregnancy. The chances of conceiving through IUI are significantly lower than that of IVF. The procedure involves injecting the healthy sperm directly into the woman’s uterus to increase the chances of fertilization and embryo implantation. IUI is scheduled around the time of ovulation.
However, if we compare the IUI vs. IVF success rate, the latter is more effective. IUI has a success rate of 5-20 percent per cycle, while the success rate of IVF is close to 45% in healthy women.