- ABOUT
- TREATMENTS & SERVICES
Male Fertility
Genetics & Family Balancing
- SUCCESS STORIES
- CONTACT
- BLOG
In-vitro fertilization (IVF) is a widely performed assisted-reproductive procedure that helps couples struggling with infertility conceive. ICSI—Intracytoplasmic Sperm Injection is a part of IVF.
The procedure involves all the steps of a standard IVF process except the fertilization. In ICSI, a healthy sperm is selected and injected into the mature egg instead of leaving it in a laboratory dish to fertilize overnight. Intracytoplasmic Sperm Injection is performed in case of male infertility or when the sperm and eggs do not fertilize naturally in an incubator.

ICSI treatment aims to increase your chances of conceiving through IVF by improving the success rate of fertilization. Here’s the step-by-step ICSI process.
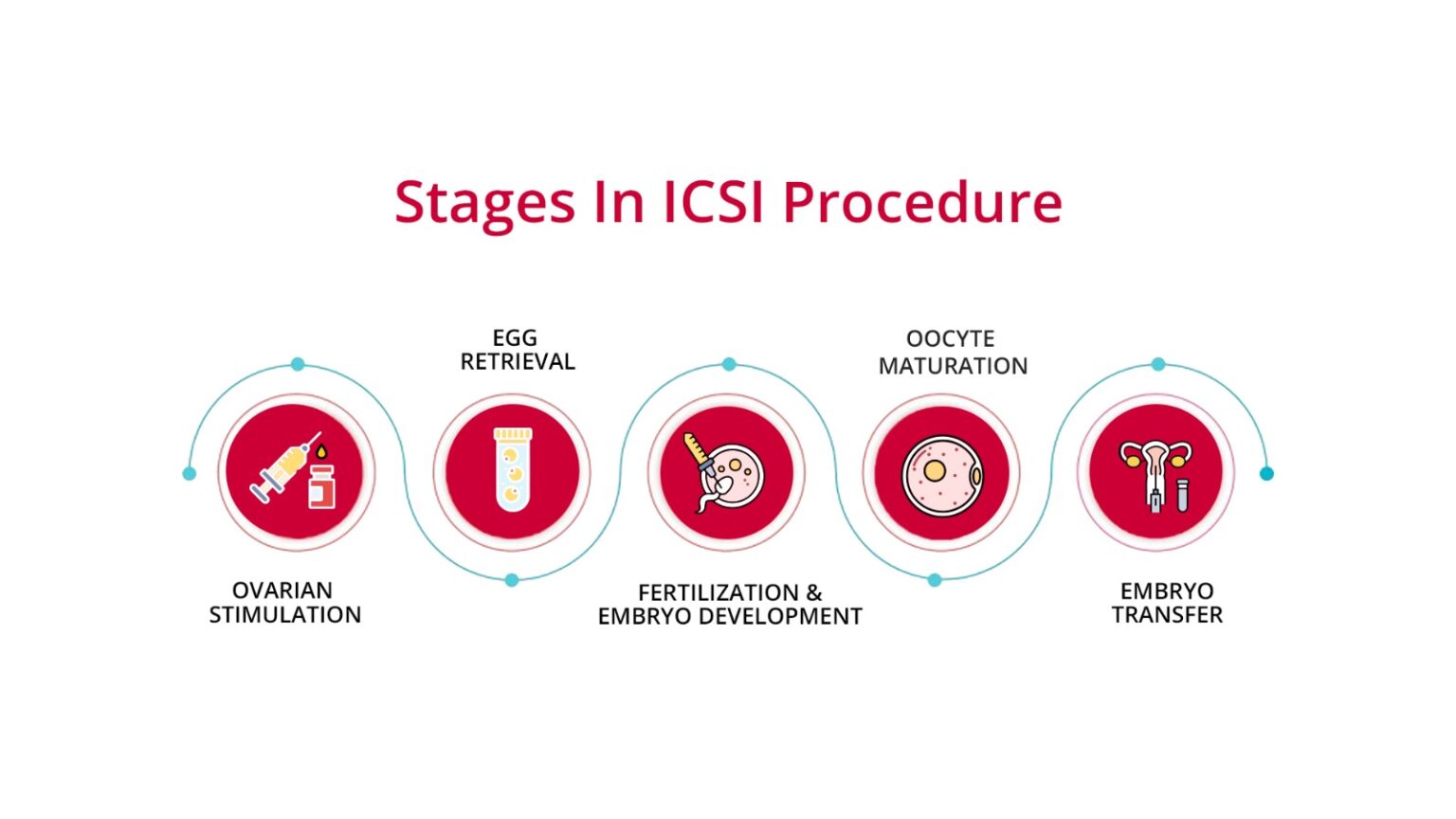
You need to take hormonal shots from the second or third day of your period for 10-12 days to release multiple mature eggs from your ovaries. In each ovulation cycle, a woman’s ovaries release one healthy egg. However, for an IVF procedure, hormonal drugs are used to retrieve multiple eggs, thus increasing the chance of fertilization.
These embryos will be put in a petri dish for 5-6 days following the ICSI procedure. The embryologist creates an environment where embryos can grow normally and reach the blastocyst stage. At this point, your healthcare provider will prepare you for the final step of the fertility treatment, i.e., the transfer of the embryo into your uterine lining.
ICSI is not performed in all IVF fertility cases. It’s needed in the case of male infertility or when the previous IVF cycles have failed. Some ICSI indications include poor-quality sperm, a genetic disorder, ejaculatory dysfunction, and failed fertilization in a standard IVF procedure. ICSI is also performed if the couple chooses PGD (preimplantation genetic diagnosis).
IVF is a fertility treatment that may or may not involve ICSI. Whether or not your case requires Intracytoplasmic Sperm Injection depends on the quality of the woman’s eggs and the male’s sperm.
ICSI treatment adds to the cost of the IVF procedure. It’s recommended only if the IVF procedure has failed. That’s because this additional step in your fertility treatment requires a suitable environment for fertilization and a professional who can carefully inject the sperm into the eggs. Besides, there’s no 100% guarantee that the procedure will fertilize all healthy eggs.
ICSI can fertilize 50-80 percent of the eggs, but like any medical procedure, there is a chance that the procedure might fail. ICSI is quite effective in increasing your chances of conceiving. However, it’s only a part of the IVF treatment.
There are many factors affecting the outcome of in-vitro fertilization, such as maternal age, genetic disorders in couples, and the mother’s reproductive health. ICSI success rate might contribute to the outcome of IVF procedures, but it alone won’t guarantee a healthy and viable pregnancy.
While ICSI improves the fertility odds in infertile partners, the procedure comes with risks. Here are some ICSI treatment risks you must be aware of.
The success rate of ICSI also depends on the IVF center you choose. Australian Concept Infertility Medical Center is, so far, the best IVF clinic in the country. They have delivered 15000+ babies through IVF and have performed numerous ICSI procedures to increase the fertilization success rate in couples who can’t conceive naturally.
ICSI is a complex procedure requiring an expert embryologist who can inject sperm into an egg and keep it in a closely monitored environment to achieve the highest success rate for fertilization. The cost of the procedure depends on the clinical or medical history of the patient
For First free Consultation Book Now!
ICSI stands for Intracytoplasmic Sperm Injection. It is a specialized form of in vitro fertilization (IVF) used primarily to treat severe cases of male infertility. During ICSI, a single sperm is injected directly into an egg to facilitate fertilization, which can then be implanted into the uterus. This technique is particularly useful when there are issues with sperm quality or quantity, such as low sperm count or poor motility.
ICSI is more effective than traditional IVF for severe male infertility, improving fertilization rates when sperm quality or quantity is an issue. For cases without significant male factor infertility, both methods have similar success rates. The choice between ICSI and traditional IVF depends on the specific infertility diagnosis and recommendations from a fertility specialist.
Male Factor Infertility: Severe male infertility issues, such as low sperm count, poor sperm motility, or abnormal sperm morphology.
Previous Fertilization Failure: Couples who have experienced failed fertilization attempts with traditional IVF.
Pre-implantation Genetic Testing: When genetic testing of embryos is necessary before implantation.
Certain Female Infertility Cases: Including poor egg quality or unexplained infertility.
The success rate of ICSI treatment in Lahore, Pakistan ranges from 50% to 80%. Specific clinics report success rates of 65% to 70%.
Kindly fill in the form below and your nearest Australian Concept Clinic will respond within 1 hour of receiving your request.
32-A, Rojhan Street, Block 5, Kehkashan, Clifton, Next to PRANZO Restaurant, Behind BBQ Tonight, Near BILAWAL Chowrangi, Karachi, Sindh, Pakistan 75600
116 Babar Block, Barkat Market, Near Salaar Center, Lahore, 54000.
3rd Floor, Aklas Plaza, G10 Markaz, Behind Babri Masjid, Sawan Road, Islamabad.
The Australian Concept Infertility Medical Center “Australian Concept” was established in 1998 with Australian technical collaboration in Karachi, Pakistan.