Myths About Infertility
MYTHS ABOUT INFERTILITY
Myths About Infertility
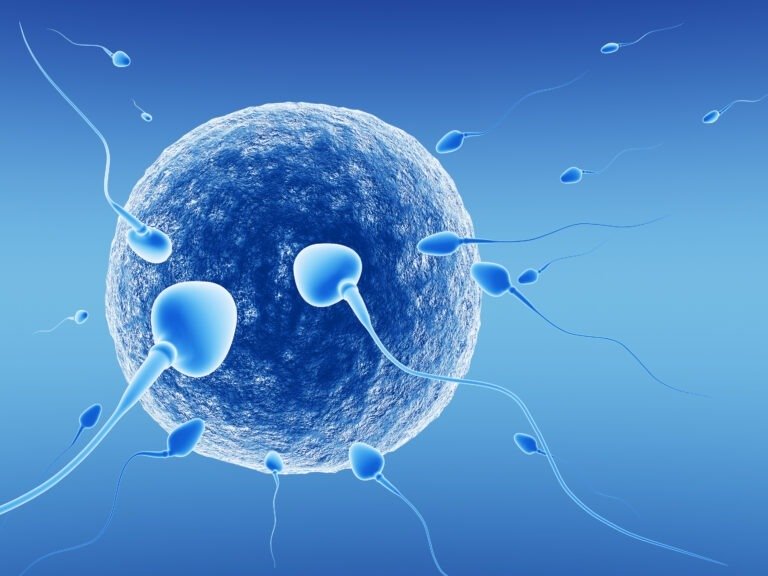
The word “infertile” means produce offspring or unable to reproduce itself. In medical terms, infertility often pertains to the inability to conceive a child despite regular unprotected sexual intercourse for a significant period. A person or a couple is said to be infertile when it is unable to conceive naturally after trying for over an year. Infertility in women declines with age therefore, for women above 35 years of age, infertility is defined as their inability to get pregnant after trying for 6 months. 1 in every 7 couples are said to be infertile. In almost half of these couples, male infertility plays a partial role at least. The lack of awareness about infertility has caused people to believe the common myths about infertility and infertility treatment.
Causes of Infertility
Infertility can be caused by numerous reasons. Sometimes, the cause of infertility is unidentifiable. 1 in every 4 couples experience unexplained infertility. The causes of infertility can be:
In women:
- Polycystic ovary syndrome
- Endometriosis
- Damaged / Blocked fallopian tubes
- Thyroid problems
- Premature ovarian failure
- Pelvic inflammatory disease
- Fibroids formation in / around womb
In Men:
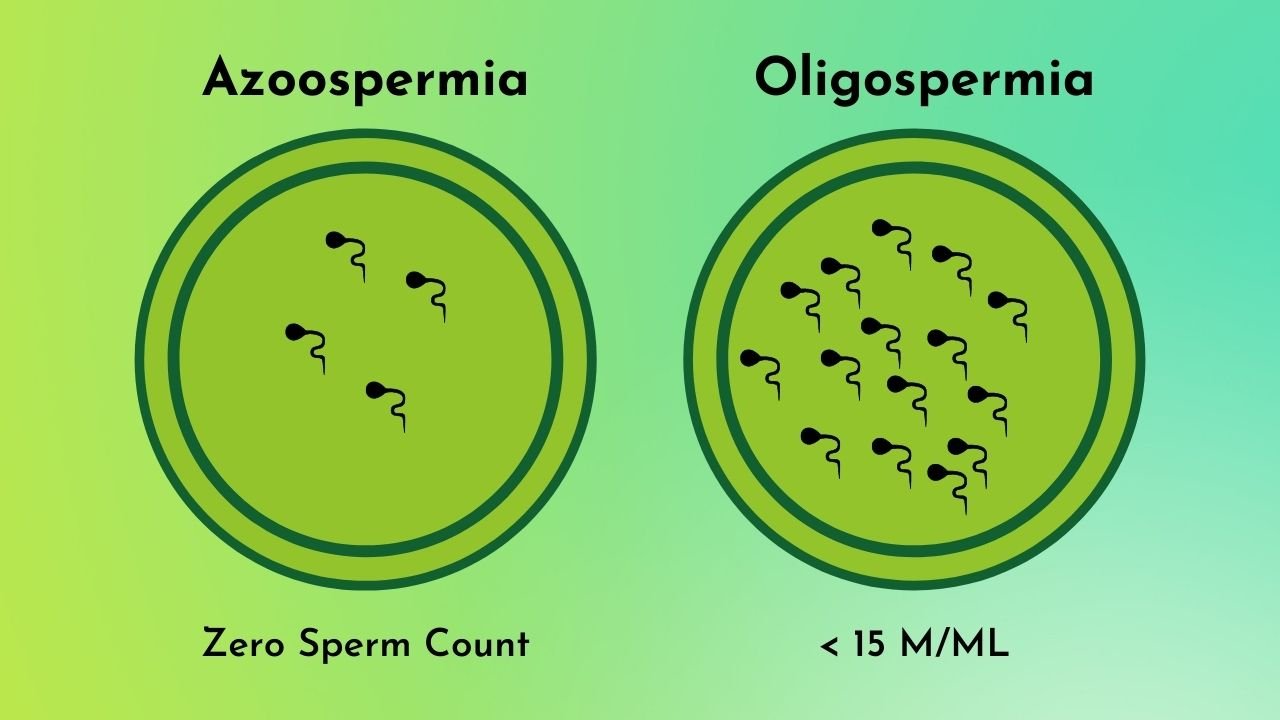
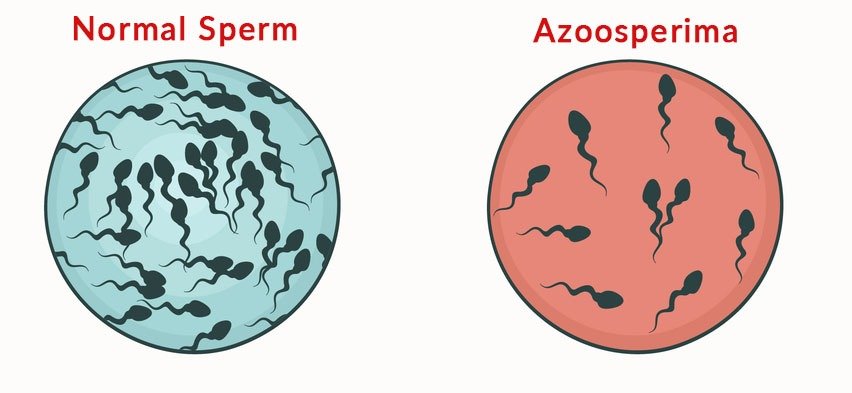
- Low sperm count
- Absence of sperm
- Poor sperm motility
- Abnormal sperm
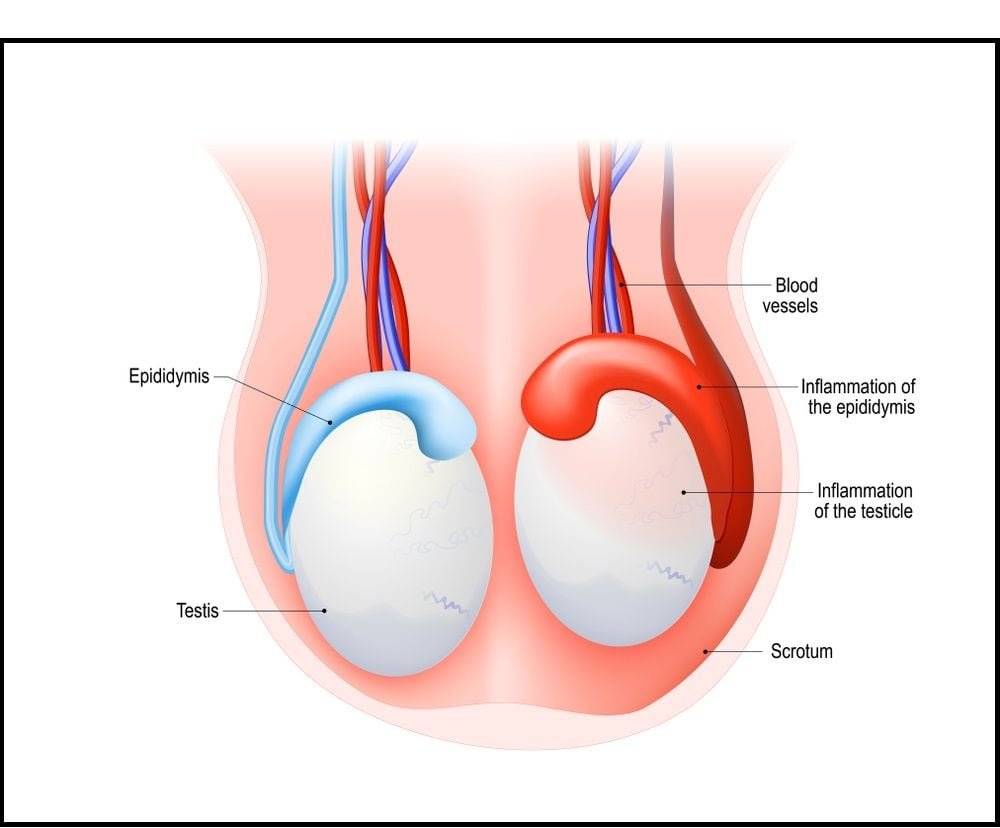
- Testicular cancer / surgery
- Injury to testicles
- Undescended testicles
In both men and women, sedentary lifestyle and drug abuse along with the side effects of certain medication can also be a cause of infertility.
Infertility Treatment
Infertility can be caused by a number of reasons but it cannot be cured. Infertility is a medical problem which can only be treated through various procedures and techniques. Following are some treatments commonly recommended for infertility treatment:
- Medication / Hormone treatment
- Surgery such as, fallopian tube surgery, and laparoscopy.
- Assisted Reproductive Technology (ART) such as, Intrauterine insemination, in vitro fertilization, etc. Before deciding to go for such treatment, people must be aware of infertility treatment cost in general, IVF treatment and successful IVF centres in Pakistan to minimise their chances of becoming a victim of misinformation.

Common Myths about Infertility
Pregnancy and infertility are two topics which are never short of myths. Most often, these myths are circulated by literate people and family who are trying to help and make people affected by it feel better. Although it is done in good faith, but it can be negative influence towards the person’s mental health during the journey. Such myths can even hold a person back from getting the care and fertility treatment he needs. Following are the five myths about infertility with facts:
Infertility is a rare condition
People assume that infertility is a rare condition and most women don’t struggle with it. Whereas, in fact, a vast number of people struggle with conception and have fertility issues. In near future, infertility can perhaps become a social issue globally. It is recommended for women below the age of 35 years to visit a doctor if they are unable to conceive after trying for over an year and for women above 35 the time period is lessened to 6 months.
Infertility is a women’s problem
People often attribute infertility with women and believe it to be a medical conditions that only affects women. In fact, infertility can impact men also. To determine the root cause of infertility, both men and women are examined and evaluated. Data reveals that almost 50% cases of infertility are due to male factors such as, low / no sperm count, abnormal sperm shape / motility, etc.
Fertility is not affected by increasing age
People have a misconception that fertility is not affected by age if you are healthy. They even believe that waiting to get pregnant can not be issue as treatments like In vitro fertilization are available. This is NOT true at all. The older a woman gets, the more struggle she will face to conceive. The quality and quantity of egg starts to decrease with increase in age at a substantial rate. Therefore, seeking early assistance in this regard can be fruitful.
Conceiving for the second time is easy
Due to lack of awareness, people tend to assume that infertility cannot affect them if they already have a baby. But the fact is, infertility is classified into types one of which is secondary infertility. Secondary infertility is a condition which affects the couple who already have a child but are unable to conceive or carry a pregnancy for a second time. The same factors causing primary infertility can cause secondary infertility also, the treatment of subsequent infertility is same as for primary infertility.
Stress causes infertility
High stress condition can cause ovulation issues but stress cannot be directly linked as a cause of infertility. Oftentimes, people in good faith, advice couples experiencing infertility to take as less stress as possible if they desire to conceive but it is so inaccurate for people dealing with it. Stress minimizing activities can have a positive impact upon the health and well-being of patients but such activities are not proven to benefit fertility.
People shouldn’t let these myths deter them from getting timely treatment. Also, men tend to believe some common myths about male infertility which are not true at all, such as:
Male fertility isn’t affected by age
Similar to women, male fertility is also affected by age in fact, the sperm quality and quantity starts to decrease after 40 years of age in men.
Men don’t need supplements to boost fertility
Like folic acid helps women in getting pregnant, it can help men in maintaining a healthy sperm count as well. Low folic acid intake is often linked with high rate of chromosomal abnormalities in sperm. Besides, Vitamin E and coenzyme Q10 also helps in this regard.
Caffeine doesn’t impact sperm count
Consuming more than 4 cups of caffeine a day can have serious effects on male fertility. As per Nutrition Journal 2017, in taking more than four cups of coffee in a day can result in abnormally shaped sperm.
Misconceptions about infertility in general and male infertility are still abound. In order to prevent yourself from becoming a victim of misinformation, you should develop an understanding of infertility and its treatments. It can prove to be immensely helpful when you’re planning to start a family.
Leave a Reply
CATEGORIES
RECENT POSTS

Myths About Infertility
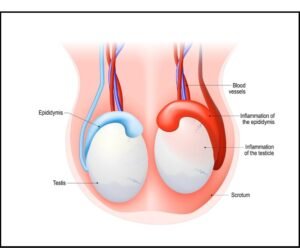
Testicular Biopsy

Fertility Treatment And Financial Planning

What is ICSI Treatment?